Beliefs not Biomechanics
Pregnancy related pelvic girdle pain (PPGP) impacts between 56%-72% of pregnant women and is a significant cause of disability, reduced quality of life and early leave from work. Physiotherapists are ideally placed to treat and manage PPGP, but some of the messages we are giving women through our language and treatments are disempowering women and increasing the pain. Here we will address how best to manage PPGP in women.

What is it?
Pain can be felt in the middle of one or both buttocks or in the pubic bone. Women will describe it like a sharp stabbing pain in the bum or as if they have been kicked right in the centre of the pubic bone.
What are the common signs of PPGP?
Pain or discomfort with:
· Turning in bed
· Going from sitting to standing
· Getting out of a car
· Pushing heavy objects, like a shopping trolley or a hoover
· Walking upstairs, or any standing on one leg, e.g. when putting on underwear
· Walking
Not just a biomechanical issue
For many years PPGP has been viewed as mainly a biomechanical and hormonal issue so treatment tended to focus on this aspect. However, as more research around pain science emerges, we now know that there are cognitive components that contribute to PGPP and its severity.
What do I mean by cognitive components?
This refers to patterns that have developed in the brain relating to current/past events/experiences, how we interpret them in our brain and whether that interpretation causes stress/anxiety.
Examples of current circumstances, past events and life experiences that impact PPGP according to the evidence are:
· Work dissatisfaction,
· Previous pelvic trauma (including traumatic birth experience)
· History of low back pain and /or PGP, especially in a previous pregnancy.
These factors have the potential to impact an associated fear which in turn impacts the level of pain through nociplastic processes (generated from the central nervous system as opposed to local inflammatory processes).
Biomechanics and hormones still play a role, just not in the way we thought. Rather than the pelvis being unstable it is more a case of the muscles/tissues surrounding the pelvis becoming more sensitive which generates protective responses and tension develops. This is felt as tightness by women and causes movements to be painful.
Also, it appears that the main hormone that can ramp up this tissue sensitivity is oestrogen as opposed to relaxin. Oestrogen significantly drops after delivery of the baby and placenta, which may contribute to why there is such a significant decrease in symptoms immediately after the birth.
How does this change how we treat and advise women with PPGP?
Now we know better, we must do better.
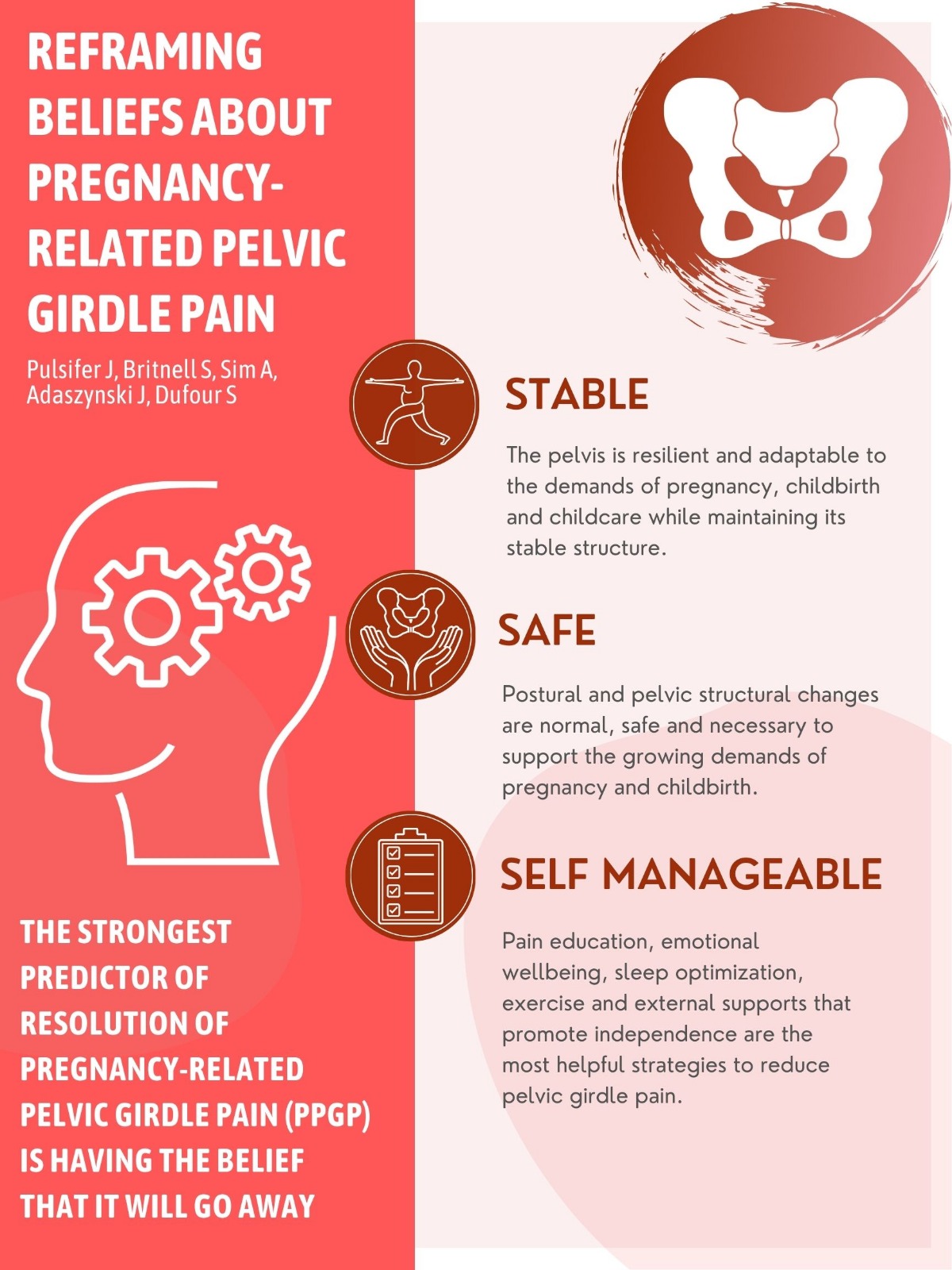
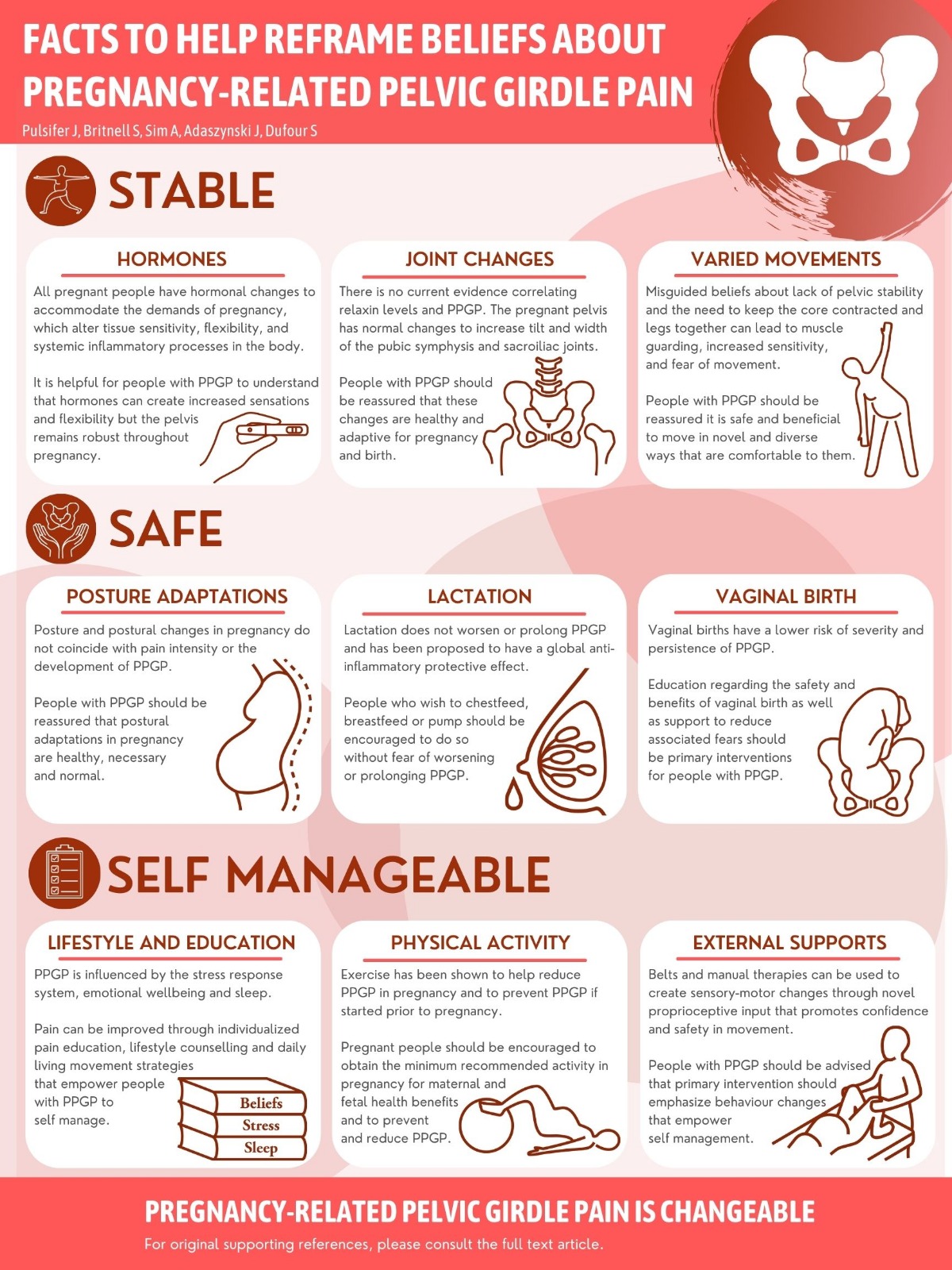
According to a recent editorial (Pulsiger et al. 2022) unhelpful narratives about PPGP that we as health care professionals need to stop feeding into are:
· The hormone relaxin makes the pelvis unstable.
· Pelvic pain is worse because of poor posture and alignment.
· Pelvic pain is caused by unstable pelvic ligaments and joints.
· Moving less and keeping the legs closed with reduce pelvic pain.
· Breastfeeding hormones will prolong pelvic pain and instability.
· Birthing vaginally will worsen pelvic pain.
· Support belts should be worn to help stabilise the pelvis.
These statements lack current supporting evidence and can contribute to unhelpful beliefs resulting in conflicting management strategies or failure to address many of the components influencing the pain.
So, what do we say to women with PPGP
Address their overall wellbeing first.
· Ask about work & home- is it stressful? what are dealing with? what type of physical/emotional support they have?
· Ask about sleep
· Ask about previous birth experience/pregnancy journey or get a sense if there are any sources of fear/anxiety
· Ask about what they do to unwind/decompress/complete the stress cycle
The intention of the above is to bring awareness to how much this woman is dealing with. Once there is an awareness this can bring acceptance and action. Action frequently requires slowing down, recognising their needs, sharing with people and asking for help to meet their needs.
Imagine if we could all do this!
Listen so they are left feeling heard, supported and validated about their experience of PPGP.
· Acknowledge everything they are currently doing before offering anything.
· Ask them what would they advise their best friend to do.
· Give them permission to slow down or stop the aspects of their lives that may be a source of stress.
· Offer tools and resources if appropriate after all of the above.
Tools and resources- provide confidence, reassurance and guidance
· NEW infographic developed by Pulsiger et al. 2022 (see below)
· SRC pregnancy leggings (https://srchealth.com/collections/pregnancy) – very supportive pregnancy leggings or shorts. There is no current evidence about the efficacity of supportive wear or belts. Feedback from women in our classes is positive. The intention is not to offer stability to the pelvis but to support the lymphatic system and provide input in the muscles/ligaments of the pelvis and legs to help reduce sensitivity.
· Mama turn (https://easiturn.com) – a great new product developed by physiotherapists in Northern Ireland to help turn in bed. Retails at £40
· Encourage tools to help reduce stress/anxiety such as gentle birthing courses/birth debriefs/emotional resilience/doula support.
· Breathing- deep breathing/meditative practices/ use of apps like headspace really help dampen down the sympathetic nervous system which reduces the central nervous system response.
· Afternoon re-boot- technique we advise in the Bump Room is resting legs upon a wall/headboard of a bed around the time they hit a slump, deep breathing for 5 mins. (see image)
· Sleeping positions- the main intention is to set women up into a position that is supportive, ideally on their side with the hip/knee/ankle along the same plain (see image). Also if the hip they are lying on gets sore to pop a towel under the sheet to offer more padding there.
· The Bump Room offers classes specifically designed for women with PGPP called Finding Relief. There is a free 40 minute video on the websitehttps://thebumproom.ie/free-resources/. In addition to a pre-recorded video library or live zoom classes.
Burnout: The secret to solving the stress cycle Emily & Amelia Nagoski
Beyond Birth: A Mindful Guide to Early Parenting Paperback ( 2021) by Sophie Burch

